Overview

Fallen arches, or flatfoot, is a condition in which the arch on the inside of the foot is flat and the entire sole of the foot rests on the ground. It affects about 40 percent of the general population. Although flat feet in and of themselves are not usually problematic, they can create problems in the feet, hips, ankles and knees. Pain may be experienced in the lower legs if there are alignment problems and if the individual is engaged in a lot of heavy, high-impact activities that put stress on the bones and muscles of the lower legs.
Causes
Genetic predisposition. Faulty foot mechanics, e.g. excessive pronation. Abnormal bony architecture. Laxity of ligaments. Neuro-muscular disease. Trauma to the leg muscles or major tendons. Inflammatory diseases of the joints e.g. Rheumatoid arthritis. Surgical procedures on the leg and ankle. Limb length inequality. Tight Achilles tendon.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
fallen arches support
Non Surgical Treatment
Some of the aspects of the pain with a ?fallen arch? are related to the crushing of the joints of the outside of the foot and from the stretching of ligaments and tendons of the inside of the foot. Unfortunately, some parts of the damage from the fallen arch, the weakness in the tendons and the new shape of the foot, are not correctable without surgical reconstruction. The first goal is to stabilize the collapsed arch. This can be done through braces. If the deformity is mild, an over-the-counter arch support may be sufficient. In more severe deformities an hinged or solid ankle brace may be necessary. Rehabilitative exercises under the supervision of a physical therapist will help increase the strength of the remaining muscles. Stiffness of certain tendons including the Achilles and hamstring is also very helpful as tightness in these structures is very common in people with ?fallen arches?. Postural training is necessary. A short period of casting or walking in a cast boot will improve swelling of a recent partial tear of the tendons and ligaments on the inside of the ankle. Nonsteroidal anti-inflammatory medications such as ibuprofen, and naprosyn can help to relieve the pain, but do not heal the injuries associated with this or decrease the swelling significantly. Surgical reconstruction is available if the pain cannot be controlled reasonably with these measures.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

Fallen arches, or flatfoot, is a condition in which the arch on the inside of the foot is flat and the entire sole of the foot rests on the ground. It affects about 40 percent of the general population. Although flat feet in and of themselves are not usually problematic, they can create problems in the feet, hips, ankles and knees. Pain may be experienced in the lower legs if there are alignment problems and if the individual is engaged in a lot of heavy, high-impact activities that put stress on the bones and muscles of the lower legs.
Causes
Genetic predisposition. Faulty foot mechanics, e.g. excessive pronation. Abnormal bony architecture. Laxity of ligaments. Neuro-muscular disease. Trauma to the leg muscles or major tendons. Inflammatory diseases of the joints e.g. Rheumatoid arthritis. Surgical procedures on the leg and ankle. Limb length inequality. Tight Achilles tendon.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
fallen arches support
Non Surgical Treatment
Some of the aspects of the pain with a ?fallen arch? are related to the crushing of the joints of the outside of the foot and from the stretching of ligaments and tendons of the inside of the foot. Unfortunately, some parts of the damage from the fallen arch, the weakness in the tendons and the new shape of the foot, are not correctable without surgical reconstruction. The first goal is to stabilize the collapsed arch. This can be done through braces. If the deformity is mild, an over-the-counter arch support may be sufficient. In more severe deformities an hinged or solid ankle brace may be necessary. Rehabilitative exercises under the supervision of a physical therapist will help increase the strength of the remaining muscles. Stiffness of certain tendons including the Achilles and hamstring is also very helpful as tightness in these structures is very common in people with ?fallen arches?. Postural training is necessary. A short period of casting or walking in a cast boot will improve swelling of a recent partial tear of the tendons and ligaments on the inside of the ankle. Nonsteroidal anti-inflammatory medications such as ibuprofen, and naprosyn can help to relieve the pain, but do not heal the injuries associated with this or decrease the swelling significantly. Surgical reconstruction is available if the pain cannot be controlled reasonably with these measures.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.




 Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.
Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.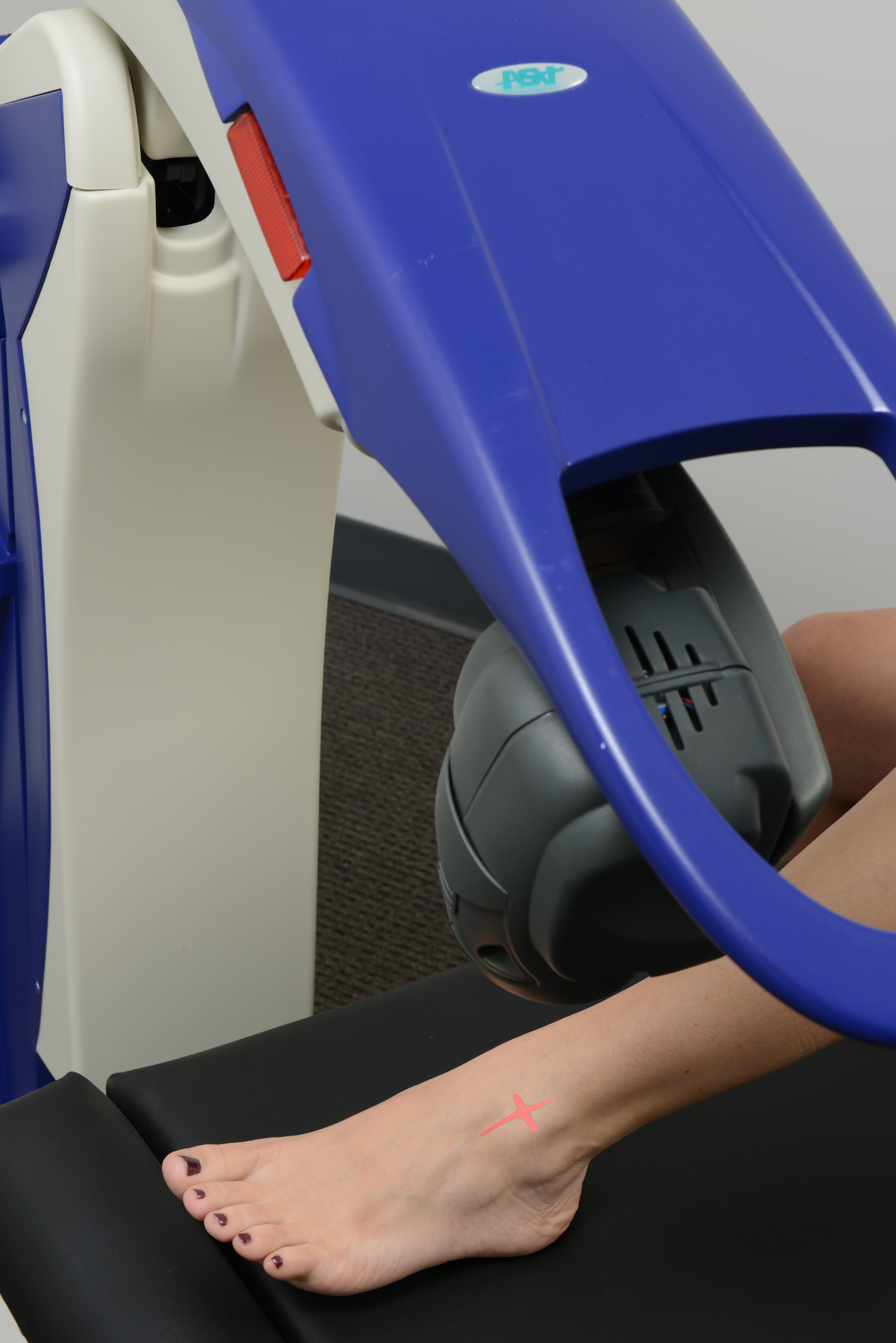






 Overview
Overview Symptoms
Symptoms Prevention
Prevention RSS Feed
RSS Feed
